Acknowledging Mental Health in the Workplace
Mental health matters. It is a critical part of every person’s quality of life. However, according to the 2021 State of Mental Health America report, over 19% percent of adults are experiencing a mental illness. That is equivalent to over 47 million Americans. And this only represents those with a diagnosis — the prevalence of mental health challenges is much higher. This is why it is very important for employers to optimize mental health in the workplace across their teams.
People with depression are at higher risk of developing other medical conditions, including cardiovascular disease, diabetes, stroke, and Alzheimer’s disease. In almost everyone, depression leads to fatigue, sadness, and problems with appetite and sleeping. Depression is more than just a bad mood; it requires immediate medical attention.
From an organizational standpoint, mental health in the workplace matters because we all care about our staff. It also matters because poor mental health has a terrible impact on productivity. In the US, 200 million workdays are lost annually due to depression, costing employers $17 billion to $44 billion. Depression is a major cause of disability, absenteeism, presenteeism, and productivity loss.
The evidence is clear: People struggle with their mental health — and it impacts every aspect of their lives.
But, if that’s the case, why aren’t more people talking about it?
Why It’s Difficult to Get Help
As a culture, we celebrate — and even reward — people for taking care of their physical health. Think about your company’s employee benefits. Your company, like many others, might offer financial incentives to employees who complete their annual physical or wellness screening. However, the same sophisticated perspective is rarely applied to mental health in the workplace.
Seeking medical attention for a physical ailment is socially acceptable. What should you do if you become ill, break a bone, or notice something out of the ordinary? You are given medical attention. Nobody thinks too much of it. We’re also usually open to discussing physical ailments. If you fractured your foot, you’d probably be fine with telling anyone from the Starbucks barista to a coworker in a crowded elevator.
But the same is not true for our mental health. In fact, estimates suggest that only half of individuals with mental illnesses receive treatment, according to the National Institute of Mental Health. People are not comfortable talking about the state of their mental health, even to their closest friend or relative. That is why it is challenging for employers to address mental health in the workplace. Fortunately, there are strategies to reduce stigma in mental health, and employers can take the initiative to do it.
Some of the barriers that prevent people from getting the help they need include:
1. Financial cost of treatment (therapy or medications) — According to the Mental Health America’s 2020 Access To Care Data report, 10.3% (over 4.7 million) of adults with a mental illness remain uninsured. Under the Affordable Care Act (ACA), the U.S. continues to see a decline in Americans who are uninsured. There was a 1.9 percent reduction from last year’s dataset.
2. Fear of being judged by others — The stigmas that surround mental health often prevent people from speaking up. Some of the misconceptions people might have about those with any mental illness is that they’re unstable, violent or a threat. This is especially true when it comes to discussing mental health in the office. As a result, people who are struggling with their mental health often suffer in silence, believing that they simply need to “toughen up” or that their problems will pass.
3. Discrimination in the workplace — Some employees might be concerned that talking about their mental health would jeopardize their jobs, even though the Americans with Disabilities Act protects against discrimination or harassment at work due to a mental health condition.
Stigma, stereotyping, and discrimination against employees with mental health problems, be it subtle or overt, can cause harm. Mentally ill people are stigmatized and discriminated against in a variety of ways, but understanding what that looks like and how to address and eliminate it can be beneficial.
Discrimination includes firing people, passing them over for a promotion, or forcing them to take time off due to their mental illness. A key reason people mention for not seeking mental health treatment or counseling, despite knowing they need it, is concern about how it will affect their jobs.
According to the Mental Health America’s 2020 Access To Care Data report, 10.3% (over 4.7 million) of adults with a mental illness remain uninsured.
Other factors that influence someone’s willingness to talk about or seek help with their mental health condition include their age demographic. The likelihood that someone will be open to discussing or seeking help for mental health in the workplace varies greatly by generation.
Gen Z is more likely than other generations to report that their mental health is fair to poor, according to the American Psychological Association’s latest Stress in AmericaTM survey. Gen Z (37 percent) and Millennials (35 percent) are both more likely to report that they’ve received treatment or therapy from a mental health professional, compared to just 22 percent of Baby Boomers and 15 percent of older adults. This suggests that there is a Baby Boomers mental health stigma.
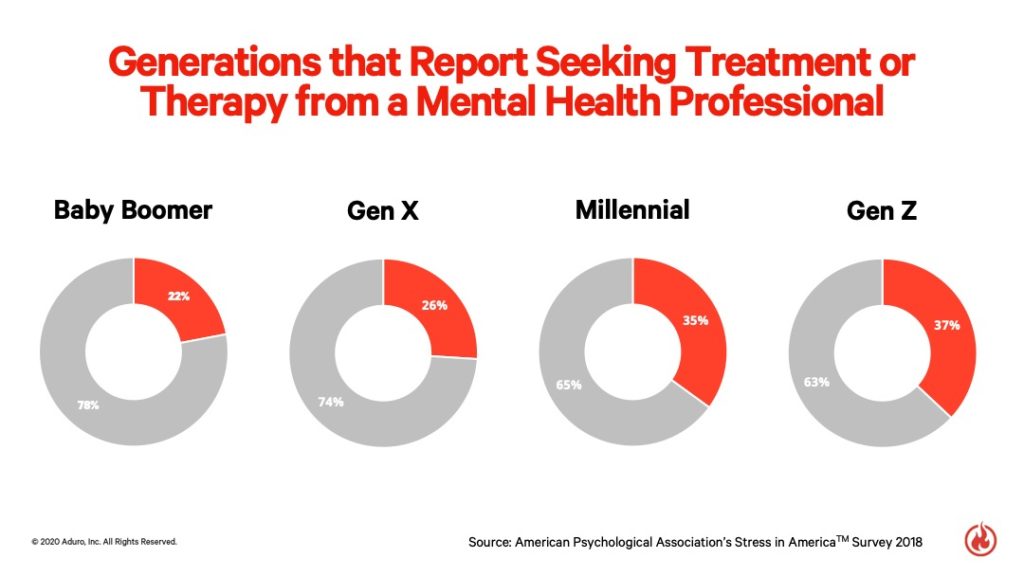
Social media may have played a role in this shift toward transparency about mental health, as Gen Z was raised in a culture that shares much more about their lives. According to a Pew Research Center 2021 study, about 71% of 18- to 29-year-olds say they use Instagram, compared to 65% for Snapchat and about 48% who use TikTok. The heavy use of social media pushes them to be more open to sharing.
The Implications of Environment on Our Mental Health
Our mental health is influenced by a variety of factors, including race and ethnicity, gender, age, income level, education level, sexual orientation, and geographic location, according to the Office of Disease Prevention and Health Promotion.
The social conditions we live in can also impact our mental health risks and outcomes.
Some of those social conditions include:
- Interpersonal
- Family
- Community
- Housing
- Social support
- Employment opportunities
- Work conditions
For employers, it’s important to recognize how a workplace’s social and physical conditions contribute to employee well-being. That’s the first step toward creating an environment and culture that promotes sustained physical and mental health.
What social and physical conditions in your workplace detract from employee mental and physical well-being? What promotes it?
Like most things in business, an important first step is getting executive buy-in.
A digital platform that helps people share social media content, Buffer, is perhaps one of the best examples of executive-level buy-in when it comes to mental health in the workplace.
Co-founder and CEO Joel Gascoigne has opened the door to talking about mental health in the workplace by Tweeting about how much therapy has helped him.
On Buffer’s company blog, Courtney Seiter, Director of People at Buffer, wrote about how Joel’s openness has helped to destigmatize the conversation surrounding mental health. She wrote that Buffer has helped normalize tears for her — and she’s so grateful for it. By allowing people to openly talk about their mental health, Buffer’s employees are able to bring their whole selves to work — without having to hide how they’re feeling.
Sometimes, talking about the darkness can help us to feel lighter, like a weight has been lifted off of our chests, allowing us to breathe again. And chances are, others can relate and even feel empowered by your humanity and openness.
Openly discussing mental health problems, including depression, can aid in breaking down barriers. Conversations help us better understand how common mental health problems are, allowing us to rectify misconceptions and feel more comfortable asking for help. All of this improves how employers handle mental health in the workplace.
Recognizing When ‘Weather Becomes Climate’
There’s a ground-breaking article entitled, “Understanding Our Own Minds,” by Jeffrey Kluger in Time magazine’s December 2019 edition. In it, Kluger talks about how there is a natural cycle in life between good and bad days. The bad days are characterized by darkness and rain, but they’re offset by good days — filled with internal sunshine. These ups and downs are normal — until they aren’t. Unfortunately, some people get stuck in a permanent down cycle.
We often do not recognize the signs soon enough, whether it’s in ourselves or others. Why? Mental health is not as black-and-white as physical health. You have a broken bone, you get an X-ray, and the results are clear. It can be difficult to recognize the difference between an employee who is going through a difficult season in life versus an employee who might be facing major depression, for example.
Fortunately, that’s where mental health professionals come in. It’s not up to employers to diagnose conditions. But it is an organizational responsibility to recognize when employees are struggling and offer ways to help.
There are even financial motivators for employers to do so.
According to the CDC, mental health and stress can impact your employees’:
- Job performance and productivity
- Engagement at work
- Communication with others
- Physical capability and everyday functioning
Nearly one in five U.S. adults live with a mental illness (51.5 million in 2019), but five in five people have mental health. It’s time to set the stigmas aside and start talking about it.